Hair loss is often seen as a cosmetic concern, but for millions worldwide, it represents a deeper emotional and psychological struggle. Among the various types of hair loss, non-scarring alopecia is both common and, fortunately, reversible in many cases. Whether you’re noticing more hair in your comb or facing sudden bald patches, understanding the causes and treatments of non-scarring alopecia can be the first step toward reclaiming your confidence.
What Is Non-Scarring Alopecia?
Non-scarring alopecia refers to hair loss where the hair follicle is not permanently destroyed. Unlike scarring (cicatricial) alopecia, where inflammation leads to irreversible damage to the follicles and permanent hair loss, non-scarring types are often temporary and treatable. The hair follicles stay unharmed, allowing the possibility for hair to regrow.
Common forms of non-scarring alopecia include:
- Alopecia Areata
- Telogen Effluvium
- Androgenetic Alopecia (Male and Female Pattern Baldness)
- Anagen Effluvium
- Traction Alopecia
Understanding which type you have is crucial for finding the right treatment.
1. Alopecia Areata: When Your Immune System Goes Rogue
Alopecia areata is an autoimmune condition where your immune system mistakenly attacks hair follicles, leading to round patches of hair loss on the scalp and other areas of the body.
Symptoms:
- Sudden, patchy hair loss
- Smooth, hairless areas on the scalp
- Tingling or burning before hair falls out
Causes:
- Genetic predisposition
- Stress or illness as triggers
- Coexisting autoimmune disorders
Treatment Options:
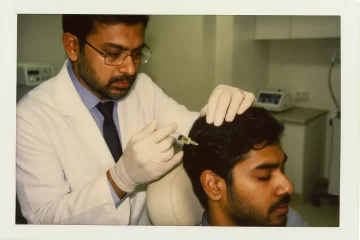
- Corticosteroid injections or creams
- Minoxidil (Rogaine)
- Immunotherapy (e.g., DPCP)
- Platelet-rich plasma (PRP) therapy
The good news? Hair often grows back, although recurrences are common.
2. Telogen Effluvium: Stress Strikes Your Roots
Telogen effluvium is a reactive type of non-scarring alopecia caused by a shock to your system—be it physical, emotional, or hormonal.
Symptoms:
- Diffuse thinning rather than patches
- Hair falls out in clumps when brushing or showering
- Onset 2-3 months after a triggering event
Common Triggers:
- Major surgery or illness
- Post-pregnancy hormonal changes
- Extreme stress
- Crash dieting or nutritional deficiencies
Treatment Approach:
- Address the root cause (e.g., improve nutrition, manage stress)
- Hair usually grows back within 3–6 months
- Supplements like biotin, iron, and zinc may help
3. Androgenetic Alopecia: The Genetic Blueprint
Androgenetic alopecia, often referred to as male or female pattern baldness, is the most prevalent type of non-scarring hair loss.
Symptoms:
- Gradual thinning at the crown and temples (men)
- Widening part or general thinning on the crown (women)
Causes:
- Genetic sensitivity to DHT (dihydrotestosterone)
- Hormonal fluctuations
- Family history
Treatment Options:
- Minoxidil (FDA-approved for both men and women)
- Finasteride (for men)
- Low-level laser therapy
- Hair transplant (for advanced cases)
Although the condition is long-term, taking early action can significantly slow its progression.
4. Anagen Effluvium: Hair Loss From the Root Up
Anagen effluvium affects hair in its active growth phase, unlike telogen effluvium, which impacts hair in the resting stage. It’s most commonly associated with chemotherapy.
Symptoms:
- Rapid, extensive hair loss
- It can affect eyelashes, eyebrows, and body hair
Cause:
- Chemotherapy or radiation
- Exposure to toxins or poisons
Recovery:
- Hair usually regrows after treatment ends
- Cooling caps during chemo may reduce the severity
- Gentle hair care and scalp massage can support regrowth
5. Traction Alopecia: Style Can Hurt
Traction alopecia develops due to prolonged tension on the hair caused by tight hairstyles.
Common Culprits:
- Tight ponytails, braids, buns
- Hair extensions
- Chemical straightening and repeated heat styling
Prevention and Treatment:
- Loosen your hairstyles
- Avoid harsh chemicals
- Use growth-supporting oils like castor and rosemary
- In severe cases, dermatological treatments may be required
Diagnosis: Don’t Self-Diagnose, Seek Professional Help
A dermatologist can help determine the type of non-scarring alopecia using:
- Scalp examination
- Trichoscopy (scalp microscope)
- Blood tests (to rule out deficiencies or autoimmune causes)
- Biopsy in rare, unclear cases
The earlier the diagnosis, the better the chances of full hair regrowth.
Natural Remedies and Lifestyle Tips
While medical treatment is often necessary, supporting your scalp health naturally can accelerate recovery:
Eat for Your Hair
- Protein (found in eggs, fish, tofu): Since hair is primarily composed of keratin—a type of protein—adequate protein intake supports healthy growth.
- Iron and zinc—found in leafy greens and nuts—help reduce hair shedding.
- Omega-3s (chia seeds, salmon): Support scalp hydration.
Manage Stress
- Try meditation, yoga, or therapy
- Persistent stress can either trigger new episodes of hair loss or extend existing ones.
Scalp Massage
- Increases blood circulation
- Promotes follicle stimulation
Natural Oils
- Rosemary oil: Proven to be as effective as minoxidil in some studies
- Castor oil: Rich in ricinoleic acid, promotes growth
- Coconut oil: Nourishes scalp and prevents breakage
When to See a Doctor?
If your hair loss is sudden, patchy, accompanied by scalp discomfort, or involves other symptoms like fatigue, weight changes, or rashes, it’s time to see a dermatologist.
Prompt action means faster recovery.
Final Thoughts: You’re Not Alone
Hair loss from non-scarring alopecia can feel like a personal crisis, but it’s a medical condition—treatable, manageable, and in many cases, reversible. From autoimmune reactions to postpartum hormone dips and lifestyle stressors, there are diverse causes behind this condition.
With accurate diagnosis, personalized treatment, and positive lifestyle adjustments, your hair can grow back stronger, and your confidence can too.